Tonsil and Adenoid Diseases
Tonsils: Tonsils are encapsulated lymph system tissues located in either side of the throat. They contain 15-20 dents (crypts) covered with lymphoid nodules (Figure 1). Tonsils may be the source of chronic infections due to the bacteria settling into the crypts that they contain and recurring acute tonsillitis episodes may occur when the resistance of the body decreases because of any reason. In addition, they may enlarge with the increase in lymph tissue due to recurrent infections and may lead to complaints like difficulty with swallowing, snoring, blocking of the air passage during sleep and apnea.
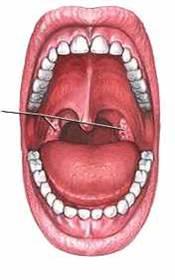
Figure 1. Tonsils
Adenoid: Adenoid tissue is located at the back of the nose, at the top of the nasopharyngeal space. It is not encapsulated and does not contain crypts (Figure 2). When the adenoid tissue enlarges and blocks the rear holes of the nasal passage, complains like nasal obstruction, snoring, apnea may be observed.
At the same time, frequently recurring adenoid infections, disrupts the function of the Eustachian tubes that open to the both sides of nasal passage and balances the pressure in the middle ear, and result in negative pressure and fluid accumulation in the middle ear (otitis media with effusion) and recurrent otitis media.
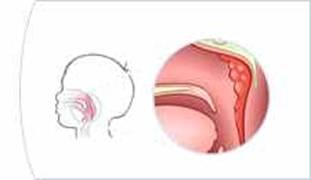
Figure 2 . Location of the adenoid tissue
ACUTE TONSILLITIS It is an acute infection of the tonsils and its severity varies according to the type of the causative microbe and the resistance of the defense system of the patient. Group A Beta Hemolytic Streptococci is the most common bacteria which causes acute tonsil infections.
Viruses (Influenza, parainfluenza viruses etc. ) also can cause similar acute tonsil infections. Viral factors are more frequent in pre-school period and bacterial factors are more frequent in adolescents and young adults. Symptoms:In acute tonsillitis symptoms start rapidly with shivering and fever, throat ache occurs. The involvement of the muscles around the throat results in difficulty in swallowing. Head ache, weakness, joints aches are present. Symptoms generally recesses in 4-6 days. Examination Findings: Enlarged tonsils with varying amounts of white membranes and inflammation in the opening places of the dents (crypts) on the tonsils are found. Hemorrhagic foci on the tonsils, reaction in all lymphoid tissues of the throat may be present. Painful lymph node enlargement in the upper neck, at the back of the corner of the chin is typical. Laboratory; White blood cells increase in blood count.
The causative microorganism is detected by examining the swab taken from the throat microscopically by gram staining, propagated in throat culture and may be shown by rapid streptococcus test.ASO, CRP and sedimentation tests are helpful in the diagnosis. The normal value of ASO is 166-200 u/dl, values exceeding these normal values are in favor of previous streptococcus infection. Treatment; Ingredients of the treatment in acute tonsillitis are;
Adequate liquid consumption,
Rest
Oral antiseptics
Analgesics, antipyretic drugs
Antibiotics: Oral treatment should at least be continued for 7-10 days. According to the order of preference;
Penicillin
Amoxicillin Clavulinic Acid
Clindamycin
Erythromycin
If the clinical findings are severe, then treatment may be initiated as intravenous or intramuscular injection, considering the difficulty in oral administration of drugs. First choice is intramuscular (IM) procaine penicillin. After continuing the treatment with 800.000 u IM two times a day in adult patients for 3-4 days, with the improvement of the clinical findings, the treatment may be completed to 10 days with oral penicillin or may be terminated by 1.200.000 u intramuscular injection with depot benzathine penicillin for once. If beta-lactamase producing bacteria are found in the environment, the response to the treatment will be reduced.
After the detection of this situation with culture, antibiogram should be performed and appropriate antibiotic administration should be started Differential Diagnosis:
Infectious Mononucleosis: This is a viral disease with Epstein Barr Virus as the causative agent. It is frequently observed during school age. The infection, known as the kissing disease colloquially, is spread by the saliva and the droplets suspended in the air.
Clinical findings are very similar to acute tonsillitis; high fever, throat ache, enlargement of the tonsils, redness and white-gray colored membrane covering the tonsils are observed. With the enlargement of the tonsils that are found in the throat, the virus spreads to the blood circulation and the liver and the spleen is enlarged. In the diagnosis, increase in cells called monocytes in the blood, monitoring the cells specific to this disease and immunological tests are used. Not having an in total white blood cell count, increase in sedimentation and CRP, elevation in liver enzyme levels, detection of enlarged liver, spleen are other findings that are helpful in the diagnosis.
The evaluation of blood smears with microscope is very important in regard to the differentiation of other blood diseases that may lead to similar findings. Diphtheria: Initiation is slow, general findings are not conspicuous. Hoarseness, shortness of breath, krup table, lymph node swelling in the throat are observed. A thick, gray membrane, tightly attached to the base is present; when removed, occurrence of bleeding is typical.
Since it releases toxins, affecting the nervous system and the heart, palpitation not compatible with fever may be detected. Diagnosis is made with Gram staining and throat culture. Scarlet fever: Tonsillitis with a thick membrane, red appearance in the tongue (strawberry tongue) occurs. Widespread swollen rash is present on the body. Diagnosis is made with throat culture and immunological tests (Dick test, Schultz-Charlton fading phenomenon). CHRONIC TONSILLITIS
Persistent inflammation of the tonsils usually develops as a result of recurrent infections. Enlargement of the tonsils, degeneration, blocking of the crypts occur. Though tonsils generally get bigger with recurring infections, sometimes they get smaller and then disappear. In chronic tonsillitis, the causative factors are the bacteria settled in the crypts. Findings:
Recurring throat aches
Enlargement of the tonsils and increase in vascularization
Foul smelling infected material accumulated in the crypts
Feverish attacks, joint pains, weakness
Swelling of lymph nodes in the throat (in active periods) becomes prominent
Treatment
Though preventive antibiotic (monthly depot penicillin injections) may be used in frequently recurring infections, generally removal of the tonsils (tonsillectomy operation) is preferred. If oversized tonsils are a big problem in children younger than the age 3, though not frequently inflamed, instead of removing the tonsils completely, their size can be reduced to relieve the air canal blockage in order to preserve their contribution on the immune system. The techniques related to this matter will be mentioned in the section on tonsil operation.
PERITONSILLAR ABSCESS Occurs as a result of spreading of the inflammation beyond the tonsil capsule. The causative factor is usually bacteria, propagating in an oxygen-free environment (anaerobic). High fever, shivering, weakness, vomiting, difficulty in swallowing, slavering, difficulty in opening the mouth, difficulty in speaking are observed.In the examination, swelling around the tonsils, edema, inflammation and membrane formation on the tonsils, are present. Edematous uvula is bended to the opposite direction. Treatment
IV antibiotic administration is initiated
It should be effective against bacteria that are resistant to penicillin (Beta lactamase producing)
Analgesic, antipyretic drugs should be administered and oral hygiene should be maintained with gargles
Emptying of the abscess
Cellulites (the period in which inflammation does not accumulate) or localized small abscess may disappear with medication
When significant amount of inflammation accumulates, it should be emptied surgically
Removal of the tonsil - Tonsillectomy (when peritonsillar abscess is present= hot tonsillectomy)
Should not be performed when severe infection findings like high fever, weakness are present
In pediatric patients when emptying and patient follow-up is difficult and in patients with frequent tonsillitis or peritonsillar abscess history, tonsillectomy may be performed following antibiotic treatment of 12 hours.
TONSILLITIS COMPLICATIONS
In tonsillitis regional infection may spread to remote regions. Pericardium inflammations (endocarditis) due to obstruction and infections of the vessels, inflammation of the kidneys (nephritis), brain abscess may develop. Respiratory tract may obstruct due to the edema forming on the larynx. Spreading to the throat and accumulation of inflammation in the throat (throat abscess), pneumonia, lung abscess, ruptures in the major veins of the neck may occur.
SURGICAL TREATMENT
Information related to tonsil and adenoid surgeries under the title Tonsillectomy and Adenoidectomy.




Comment
Your Contact Information will not be shared in any way. * Required Fields